Optimal asthma control: time for a new target
Day-to-day asthma treatment is widely based on a stepwise approach where care can be ‘stepped up’ to control symptoms, and ‘stepped down’ after a period of symptom control. We have written a review of potential problems with this approach.
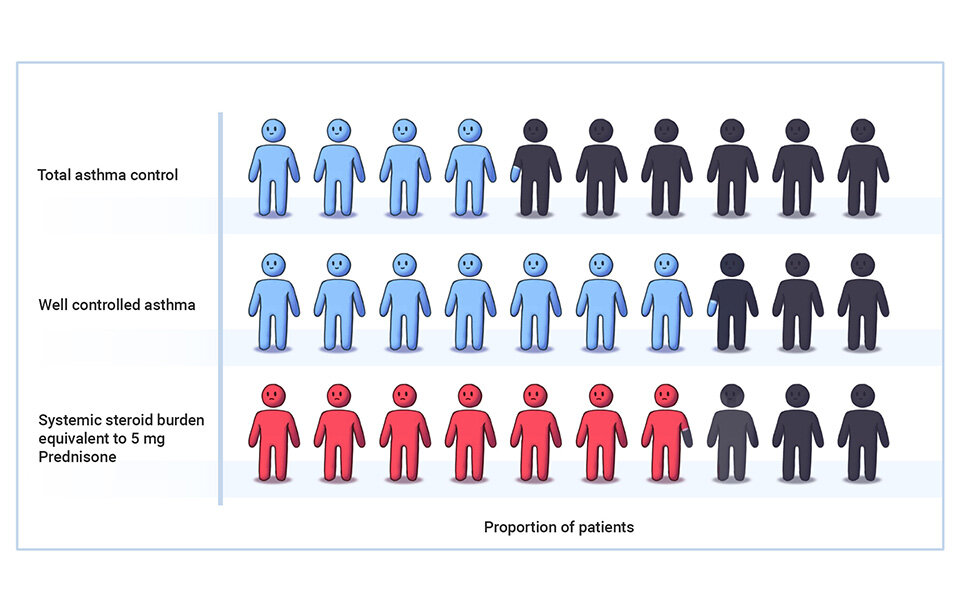
Firstly, this model can only achieve ’total control’ of symptoms for 4/10 patients, or ‘well-controlled’ symptoms for 7/10 patients, and comes at the expense of high dose inhaled steroid treatment. Given that 80-90% of the maximum obtainable effect of these medicines is achieved at low doses, there is evidence that current practice results in inappropriately high doses of inhaled steroids for many patients.
A stepwise treatment algorithm resulted in ‘total asthma control’ for about 4/10 of patients, or ‘well-controlled asthma’ for 7/10 patients. These results came at the expense of a significant steroid burden.
It is important to consider other disorders which may be contributing to respiratory symptoms in a patient with asthma, and which may need investigation and treatment in their own right. Managing other conditions a patient has (e.g. chronic sinusitis ), a condition which mimics asthma (eg COPD), lifestyle (e.g. smoking), and environmental factors (e.g. mould at home), can often improve outcomes without the need to change asthma medicines.
80-90% of the maximum obtainable effect of inhaled steroids is achieved at low doses. Figure used with permission from Professor Beasley: source paper
When patients fit a medical definition of only ‘partially-controlled’ asthma, they still report a very high quality of life and minimal impairment. This presents an important question: are our current treatment aims of tighter control relevant to our patients’ lives?
Managing other disorders which can mimic asthma (e.g. COPD) can often improve outcomes without the need to change asthma medicines. Medical illustration by Dr Ciléin Kearns
Finally, as asthma symptom control doesn’t directly reduce the risk of asthma attacks, we suggest it may be time to aim for more relevant treatment goals, such as controlling the underlying disease process of airway inflammation.
If you have institutional access, you can read the full paper in the American Journal of Respiratory and Critical Care Medicine here: http://bit.ly/Optimal-Asthma-Control